
- This event has passed.
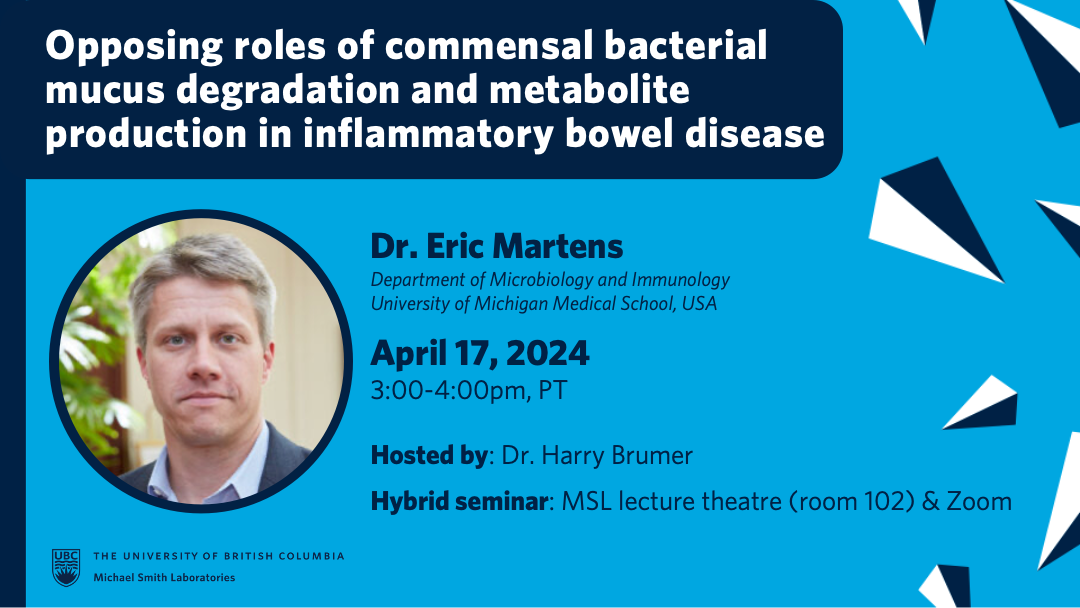
MSL Seminar Series: April – Invited Speaker, Dr. Eric Martens
April 17, 2024 @ 3:00 pm - 4:00 pm
Invited Speaker:
Dr. Eric Martens
Department of Microbiology and Immunology, University of Michigan Medical School, USA
This seminar will be presented in a hybrid format. Audience members are welcome to attend either in person at the MSL lecture theatre (room 102) or via the zoom link. Those connecting via zoom will be able to ask questions during the Q&A portion using the chat function.
Host: Dr. Harry Brumer
Zoom registration link: https://ubc.zoom.us/meeting/register/u5clc-2rqjwpEt08cz-bLQns6AsWoUjkCUVy
Talk title: Opposing roles of bacterial mucus erosion and metabolite production in inflammatory bowel disease
Abstract: Bacteria and other microorganisms that compose the human gut microbiome play positive and negative roles in several diseases. Hundreds of genetic polymorphisms have been associated with predisposition to inflammatory bowel disease (IBD), but the mechanistic roles of diet and microbiome in precipitating inflammation in genetically susceptible hosts are largely unknown. We have elucidated pro- and anti-inflammatory contributions of the gut microbiome and dietary fiber—a broad class of mostly plant derived polysaccharides—in mice lacking the anti-inflammatory cytokine interleukin-10 (IL-10-/-). When deprived of dietary fiber, some gut bacteria resort to foraging on host mucus, leading to lethal colitis in IL-10-/- mice. Selective removal of mucus-degrading bacteria abrogates colitis, suggesting the requirement of mucus erosion for disease development. Likewise, genetic elimination of the mucus layer by deletion of the host gene (Muc2) that encodes the dominant secreted colonic mucin results in disease in mice fed a high fiber diet. Different disease severity develops in mice carrying human gut bacteria compared to those with a native specific pathogen free microbiota, further suggesting specificity of microbiota effects on host. When mice with human gut bacteria are weaned onto a low-fiber Exclusive Enteral Nutrition (EEN) diet often administered to IBD patients, IL-10-/- mice present less severe colitis than mice weaned onto the disease-promoting fiber-free diet. The microbiomes of EEN-fed mice revealed unexpected expansion of the non-mucin degrading, butyrate producer Eubacterium rectale and increased levels of the branch-chain fatty acid isobutyrate. Mice fed a disease-promoting fiber-free diet supplemented with isobutyrate develop less disease, suggesting that EEN reduces inflammation by supporting protective, isobutyrate-producing bacteria that counteract inflammation caused by mucus erosion. Eliminating E. rectale from the community eliminates elevated isobutyrate production. Our results highlight the concept that microbial functions should be the focus of positive and negative impacts in the development of IBD. Some of these functions (e.g., mucus degradation) can be genetically very complex and difficult to predict from taxonomic or metagenomic data, necessitating the use of simplified systems in which function can be discovered prior to investigating roles in humans. Thus, our study provides a potential path towards leveraging features of the IBD landscape that can be intentionally manipulated (diet & microbiome) to reduce the disease burden in people suffering from IBD.