Newsroom
UBC scientists sequencing the genomes of Canadians with COVID-19
For years, genome sequencing has helped scientists better understand the factors that predispose humans to disease. Now, the tool is being used in the fight against COVID-19.
Through the Canadian COVID Genomics Network (CanCOGeN)—a new initiative launched by Genome Canada and backed by $40 million in federal funding—scientists across Canada are collaborating on genomics-based research to find solutions to COVID-19.

Dr. Terry Snutch
Among those involved are UBC’s Dr. Terry Snutch and Dr. Steven Jones, both professors in the faculty of medicine. Dr. Snutch, professor in UBC’s Michael Smith Laboratories and Djavad Mowafaghian Centre for Brain Health, is leading the $20 million COVID-19 genome sequencing component of the initiative, called CanCOGeN-VirusSeq. Meanwhile, Dr. Jones, who is co-director and head of bioinformatics at Canada’s BC Michael Smith Genome Sciences Centre (GSC) at BC Cancer, is leading the B.C. branch of the CanCOGeN-HostSeq team to sequence the genomes of 10,000 Canadians who have tested positive for COVID-19—an initiative supported by another $20 million investment from the federal government.
In this Q&A, Drs. Snutch and Jones discuss how their findings could lead to better assessment and treatment of the most vulnerable COVID-19 patients.
How can genome sequencing help scientists better understand COVID-19?

Dr. Steven Jones
TS: By determining SARS-CoV-2 genome sequences, we can easily identify small mutations, or variants, that arise as the virus is generating billions of copies of itself. By following the trail of these variants as they appear in patients across different regions, we can determine where that variant originated and, combined with that person’s travel history, when it was introduced into the region. This is crucial to distinguishing between infections arising from travel versus community spread and provides health authorities with critical information towards recommendations regarding outbreak control and where to direct resources.
SJ: We know that COVID-19 affects people differently. Seniors and those with other diseases tend to have worse symptoms and outcomes compared with young and healthy people. But some young and otherwise relatively healthy people are also seriously affected. By assessing people who have tested positive for COVID-19, and comparing the genomes of those that have responded poorly to infection to those who responded relatively well, we can tease out differences in genes that may indicate why people respond to the virus differently.
What implications could this have for the development of treatments and vaccines?
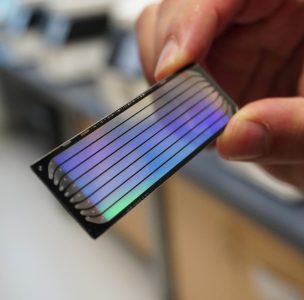
A flow cell, the site where DNA sequencing takes place.
(Photo credit: GSC)
SJ: Although we did not sequence this particular virus (laboratories in China did shortly after its initial discovery in Wuhan), UBC researchers were the first in the world to sequence a related virus, SARS-COV-1, that was responsible for the SARS epidemic in 2003. We know from that work that understanding the sequence of the virus genome can accelerate the process of finding a vaccine.
TS: The virus genome codes for about two dozen proteins. By chance, some mutations will arise spontaneously in proteins that are currently targeted for vaccine development. It is crucial that we identify and understand how viral mutations appear in vaccine-targeted proteins. If the virus mutates at a critical targeted site, a vaccine that took months or years to develop might only be partially effective by the time it is available to the public.
What do you hope comes from this work in addressing COVID-19?
TS: On the genome data side, I hope that the effort will evolve into the collective Canada-wide ability to track the virus in near real time (e.g., 24-48 hours) thus becoming an invaluable tool towards COVID-19 surveillance as new outbreaks arise and the predicted second wave appears. I also hope that the viral genome data will allow us to predict and track the development of viral resistance to therapeutics treatments.
SJ: The genes associated with outcomes for COVID-19 are part of a complex puzzle. We think there is a genetic connection associated with disease trajectory and outcome, but we won’t know the extent of that until we complete this study analyzing the genomes of people affected by the virus. The studies that come from this work will tell us a lot more about the genetics of viral infections. While we don’t know the immediate impact the current COVID-19 pandemic, we intend to be better armed with knowledge of the behaviour of this virus, which will help us to be better prepared for future pandemics.
Project collaborators include Dr. Richard Harrigan, professor in the UBC department of medicine, Dr. Marco Marra, head of the UBC department of medical genetics and director of Canada’s Michael Smith Genome Science Centre at the BC Cancer Research Institute, and Dr. Naveed Aziz, chief administrative and chief scientific officer at CGEn.
This story was originally published by the UBC Faculty of Medicine