Newsroom
Improving CAR T-cell manufacturing: Findings from the Piret lab
Dr. James Piret (left) and Dr. Alina Kunitskaya (right).
A study from Dr. James Piret (MSL, Chemical and Biological Engineering) and recent MSL and School of Biomedical Engineering graduate Dr. Alina Kunitskaya will help facilitate the manufacturing of CAR T cells by expanding the range of manufacturing conditions that can be used when the cells are at high concentrations. By offering new options for manufacturing, these improvements can reduce biomanufacturing costs and increase the accessibility of this treatment option for patients.
CAR T cells and manufacturing
Since 2017, chimeric antigen receptor (CAR) T cells have saved the lives of tens of thousands of blood cancer patients after all other available treatment options had failed.
To treat a patient using this therapy, their T cells are isolated and genetically engineered to display a receptor that will increase their binding to cancerous blood cells. The engineered CAR T cells are then multiplied in culture and injected back into the patient, where the cells perform their immune function of killing cancer cells. By bioengineering the cells, their numbers and cancer cell targeting abilities are significantly improved, which leads to the improved clinical outcomes of these therapies.
Other cancer cell types are more difficult to treat in this way, but the success of the CAR T-cell therapies for blood cancer treatment has stimulated worldwide efforts to develop similar cellular therapies for more types of incurable cancers. One challenge, however, for any therapy like this, is the high cost of manufacturing the cells. This is why engineers are working to better understand and optimize the CAR T-cell biomanufacturing process.
Filling a knowledge gap by studying concentrated cells during manufacturing

Plates of T cells are placed in an incubator that mimics the body temperature of 37 degrees Celsius.
At many steps during the manufacturing of these T cells, they are highly concentrated for processing. This includes steps where they are transitioned between different media, when they are being prepared for reinfusion into the patient, and when there are unexpected delays in manufacturing. This creates a new environment of interest for these cells, and previous studies haven’t investigated how long and at what range of temperatures these T cells can be kept at high concentrations without losing their cancer fighting abilities. A recent publication, and a large part of Kunitskaya’s PhD project, aimed to fill this knowledge gap.
“We took those concentrated cells and analyzed the levels of pH, glucose, oxygen and lactate under a range of temperatures for various time ranges of up to 6 hours, to understand how the extremely harsh conditions generated might impact cell survival, cell quality, and their function,” explains Kunitskaya.
Specifically, they tested the concentrated cells at 4°C (standard fridge temperature), 20°C (room temperature) and 37°C (human body temperature). While one might think the cells would thrive at body temperature, cells are often transported at 4°C, and so their study noted, unsurprisingly, that their best outcomes occurred at this cooler temperature.
However, it can be costly in the manufacturing environment to have refrigeration equipment for this purpose. With this in mind, their study was also able to show that cells could be kept at room temperature for 3 hours, while ruling out 37°C as a storage option since many of the T cells died or were severely deteriorated in quality.
As Kunitskaya notes, though, “There are many variations in the manufacturing process in terms of timing, media used, and other factors. This study is meant to be a guide for the temperatures these highly concentrated cells can tolerate, and for how long, but different processes might have their own optimal conditions.”
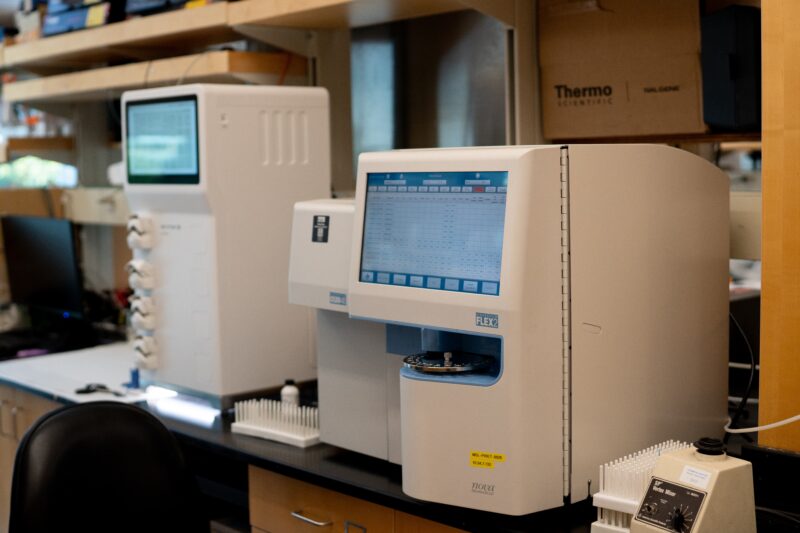
The FLEX2 instrument can analyze multiple cell culture parameters at once (e.g. glucose, lactate, pH), helping in this study to characterize the environment of the concentrated T cells.
The impact on treatment and patient outcomes
This study contributes towards the larger goal of optimizing the entire manufacturing process for CAR T cells, as this can have a significant impact on cost, and in some cases treatment success for patients undergoing the therapy.
Kunitskaya explains that the biomanufacturing of these CAR T-cell therapies for each patient is often a one-time opportunity. “If we don’t succeed in manufacturing their CAR T cells on the first try, there’s usually not another chance to try again.”
Medical science can make great advances by developing impactful therapies, but it is crucial for these treatments to be made widely available. This is why it is important for applied scientific research to focus on developing more economical and flexible bioprocessing methods, making these treatments more cost effective, and therefore accessible, to more patients.