Newsroom
The Jefferies lab discovers cannabinoids that could be used in metastatic cancer treatment
Immunotherapy is revolutionizing oncology, yet current approaches have only minor impacts on treating many types of high-grade metastatic tumours. Researchers from the Jefferies Lab at the Michael Smith Laboratories, in collaboration with the Andersen Laboratory in UBC’s Department of Chemistry, have revealed a highly significant connection between cannabinoids and potential cancer treatments. Already used to help alleviate side effects from chemotherapy, relieve chronic pain and treat a variety of other diseases, this discovery about the medicinal use of cannabis-derived compounds could greatly impact the treatment of metastatic cancers. The team has isolated specific cannabinoids that help the body revive its immune response to metastatic tumours, which typically evade our killer T lymphocytes. These immune cells are a type of white blood cell that protect against disease, infection and tumorigenesis (the creation, survival and spread of tumours).
“This is a really great opportunity to implement natural derivatives that can assist immunotherapies for treating metastatic cancers,” explains lead author, graduate student Sarah Dada.
Notoriously difficult to treat and control, metastatic cancers spread from the primary source throughout the body via the bloodstream or lymph system. They generally evolve to evade the body’s adaptive cellular immune response, which would typically trigger T lymphocytes to fight against the tumour. Metastatic cancer cells accomplish this by downregulating surface molecules on the cancer cells that flag them as tumours to our immune system, essentially rendering the cancer cells invisible.
“Cancer treatments often have different modes of action. We’re constantly trying to find new treatments that improve patient outcomes. Combining multiple therapeutic approaches can overcome tumour resistant to any individual treatment,” says Dada.
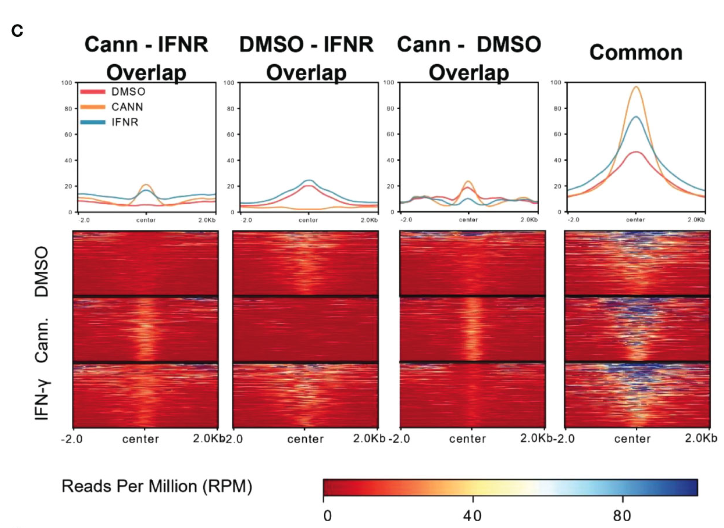
Cannabigerol induction demonstrates increased global acetylation similar to IFN-γ; IFN-γ is known to cause the increase of the MHC molecule that causes T-cell killing of cancers.
Through screening various monomolecular cannabinoids to identify promising compounds, Dada and the lab have isolated a component of cannabis that effectively removes the cloak of tumour invisibility, and thereby revealing metastatic tumours to the immune system, which can then better seek and destroy tumours.
“Immune-cloaking is common in many types of metastatic tumours. If the immune system can’t see the cancer, it can’t kill the cancer. So, our work is important for reviving T lymphocyte immune surveillance that is at the heart of many immunotherapies,” says Dada.
In the lab, researchers selected specific cannabis isolates based on their initial effect on cancer cells in test tubes and explored how the isolates affected the cancer cells. Next, they confirmed these findings with the selected cannabinoids in animal models. By successfully increasing the number of “tumour-flags” molecules on the cancer cells, the immune system could identify and attack these cells.
“Helping the body’s immune system to recognize and destroy metastatic cancers is a hugely impactful way to approach the problem. There are likely fewer side effects to aiding your body’s immune system fulfilling its normal function. The approach we describe could be another tool for people with metastatic cancers that are untreatable with the therapies that are current available” Dada explains.
This is a promising discovery that provides a molecular explanation for the reported medicinal anti-cancer effects of cannabinoid-containing plants and may catalyze the development of an effective treatment for metastatic cancers that evade the immune system. Empowering our bodies to identify and kill these cancerous cells would be a significant step forward in providing new treatment options.
Quick links:
- Read the Frontiers in Immunology publication: Specific cannabinoids revive adaptive immunity by reversing immune evasion mechanisms in metastatic tumours
- Learn more about the Jefferies lab
